“When my period comes, not only does my stomach hurt, but my head also becomes very painful,” Yuling told her colleague, “Just now, I seemed to see a flash of white light.”
“My child, who is already in puberty, experiences the same thing,” the colleague replied, “On the day her period is about to start, she can’t go to school and has to stay in a dark room because everything seems too stimulating.”
“That sounds worse than me,” Yuling asked, “Did you take her to see a doctor?”
“Yes. The doctor said it’s a hormone-related migraine,” the colleague said, “I feel so sorry for my child every time I see her in discomfort.”
Menstruation and Headaches
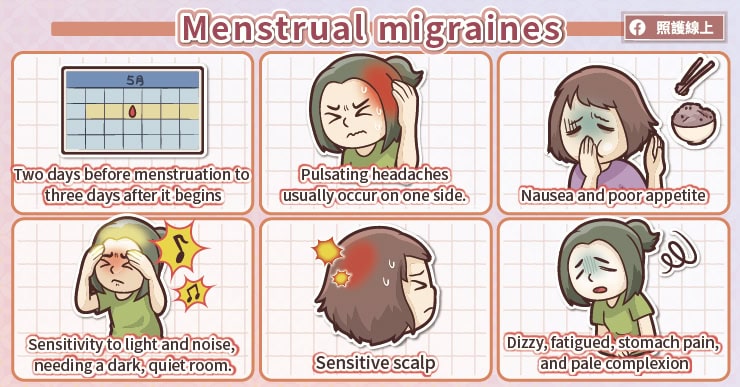
Women are more affected by migraines than men, with the number of female migraine sufferers being about three times that of males. Migraines are particularly common in women around the age of 30 and often occur around the time of menstruation. These headaches can happen two days before menstruation to three days after bleeding starts. They are characterized by a throbbing pain that can last from several hours to about a day, usually occurring on one side of the head. Accompanying symptoms include nausea, changes in appetite, and increased sensitivity to sound, light, and smells. Sensitivity to light and noise is common, and symptoms often improve when staying in a dark and quiet room. Some people may experience abnormal skin pain, where even light touches to the scalp feel sensitive. They may also feel dizzy, fatigued, have stomach pain, and appear pale.
Causes of Menstrual Headaches: Decreased Estrogen
Estrogen and progesterone are the two main sex hormones in women. For females who have reached puberty and have not yet gone through menopause, estrogen levels fluctuate. Estrogen levels are lowest during menstruation and highest in the middle of the menstrual cycle.
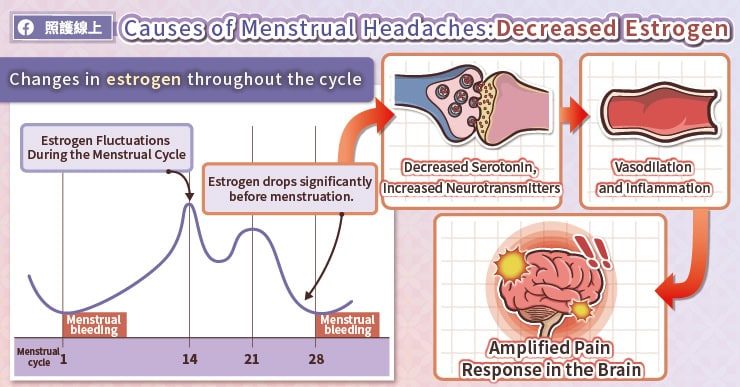
Menstrual headaches are closely related to the decrease in estrogen levels. The reason behind this is that estrogen levels are linked to serotonin levels. Before menstruation, as estrogen levels drop, serotonin levels also decrease. This increase in certain chemicals in the blood that stimulate nerves and dilate blood vessels in the brain causes migraines and can also lead to inflammation of blood vessels. Moreover, during menstruation, pain responses in the brain are amplified, making women more prone to headaches.
Similar Conditions to Menstrual Migraines
Since menstrual migraines are caused by a rapid decrease in estrogen levels, similar headaches can occur when estrogen levels fluctuate significantly, not just during menstruation.
For example, patients who need to have their ovaries removed due to illness may experience headaches post-surgery. After childbirth, estrogen levels drop rapidly, leading to hormone-induced headaches. Some people who never had menstrual migraines may start experiencing headaches after beginning to take birth control pills. During menstruation, when no pills or only placebo pills are taken, estrogen levels in the blood drop significantly, which can cause headaches. Additionally, during the pre-menopausal period, estrogen levels fluctuate, triggering headaches. Stress-induced tension headaches are also common during this time, adding to the pain.
Do You Need to Get Checked?
Currently, there are no tests that can directly diagnose migraines. Doctors need to make a diagnosis based on patient descriptions and neurological exams. If necessary, imaging or EEG tests may be arranged. Studies have shown that most patients with menstrual migraines have normal neurological imaging, with only a few showing mild brain edema or excessive cerebral blood flow on MRI.
Therefore, it is usually unnecessary to get checked every time you have a headache. However, if the nature, duration, or location of the pain is significantly different from previous headaches, you should see a doctor and consider imaging tests. Keeping a headache diary to record the time, severity, and pattern of your headaches, along with any accompanying symptoms, can help in understanding your headache patterns.
Improving Menstrual Migraines
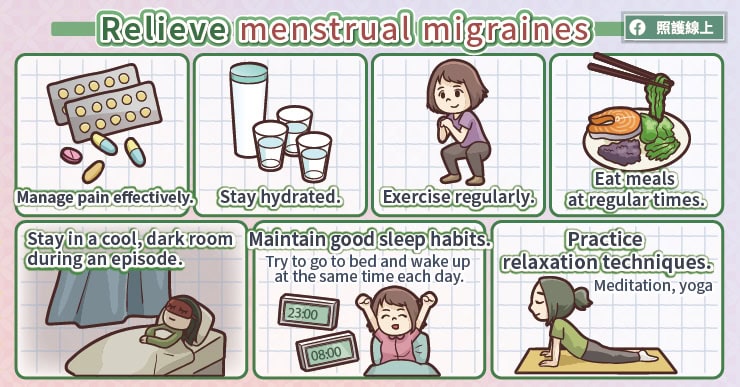
The primary treatment is pain relief. When a migraine occurs, staying in a cool, dark room can help. For those already taking oral contraceptives, adjusting the estrogen content in the medication or switching to progestin-only options may be necessary. There are various treatment options available, so it’s best to discuss them with your doctor.
For migraine sufferers, maintaining good sleep habits and quality is crucial. Try to go to bed and wake up at regular times, and develop a regular exercise routine. Stay well-hydrated, drinking about eight cups of water a day to avoid dehydration. Eat regular meals to prevent blood sugar fluctuations. Consider learning relaxation techniques like meditation, yoga, or tai chi, and opt for a lifestyle that minimizes stress.